I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
You can find the entire real patient clinical problem in this link here.
Following is the view of my case-
A 59 year old male patient came to the opd with the chief complaints of shortness of breath since 4 months and abdominal distension since 2 months.
History of presenting illness-
The patient was apparently asymptotic 4 months ago when he developed shortness of breath which was insidious in onset nd gradually progressive .
-initially it was on walking but later progressed to ordinary physical activity like bathing-NYHA -grade 3
-history of abdominal distension since two months which was insidious in onset and gradually progressive to the present size
History of bilateral pedal odema of pitting type since two months upto the knee
-history of constipation since 1 week
-NO history of fever, cough,orthopnea,chest pain,syncope,palpitations,vomitings,abdominal pain,loose stools,fever,burning micritrution,decreased urine output
Past history-
Known case of -DM-type-2 since 15years
Medication-metformin-Bd
-insulin-25units -bd
K/c/o HTN since 5-6 years (Clinidipine 20 mg BD)
H/o Tuberculosis 6 years ago - used ATT for 6 months.
Personal history
Mixed diet
Loss of appetite since 4 months
Bowel movements - irregular (alternate days)
Sleep - adequate
Addiction - Consumes 90 ml of alcohol twice a week since 25 years, stopped one year ago.
No known allergies.
No significant family history.
General Examination
Pt. Is conscious, coherent, cooperative.
Pallor +
B/L pedal edema + (pitting type, upto knees)
No signs of icterus, cyanosis, clubbing, generalized lymphadenopathy
Vitals
PR - 84 bpm
BP - 140/80 mm Hg
RR - 18 cpm
Temp- 98.4 F
Weight - 81 kgs
Height - 175 cms
BMI - 26.4
Head to toe examination
Lipodystrophic pear shaped body
Frank sign +
Mallempati Grade III
Gynecomastia +
Diabetic dermopathy +
Systemic Examination
PA
Inspection
shape of the abdomen - obese
Inverted umbilicus
No scars, sinuses, engorged veins
Palpation
no local rise of temperature, no tenderness
Consistency - Soft
Liver & Spleen - not palpable
Abdominal girth - 110 cm
Auscultation
Bowel Sounds heard
CVS
S1, S2 heard.
Feeble apex
Palpable P2
Pansystolic murmur accentuated with inspiration along left sternal border (Grade I - II)
CNS
Reflexes. Right. Left
Biceps. 2+. 2+
Triceps 2+. 2+
Knee. 1+. 1+
Ankle. absent. absent
Plantar. Flexor. Flexor
RS
Lungs - clear on auscultation, BAE +
No added sounds
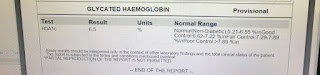
Investigations :
Chest X ray PA view





Comments
Post a Comment