Short case for practical exam
A 25 year old female patient , tailor by occupation, hailing from Thummelagudam, came to the OPD at 7.30 am with chief complaints of vomiting and loose stools since 3 am the previous night.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic few hours back when she developed vomiting- 20 episodes, sudden in onset, non bilious, non projectile, with mainly water as content.
It was associated with burning type of pain abdomen involving all the quadrants.
Also associated with loose stools- 6 episodes, watery in consistency, not associated with blood or mucus.
H/o burning micturition since 3 days.
No h/o fever and intake of food from outside, decreased urine output.
Past History:
History of similar complaints 1 year back.
History of Urinary tract infection- 3 episodes in the last 8 years.
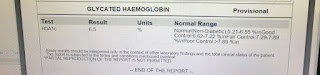
Not a known case of Diabetes melitus, hypertension, TB, Asthma, Epilepsy.
Surgical History: 2 previous LSCS
General Examination:
Patient is conscious, coherent, co-operative.
Moderately built, moderately nourished.
Pallor - present
Icterus- absent
Cyanosis- absent
Clubbing- absent
Koilonychia- absent
Lymphadenopathy- absent
Edema- absent
Vitals:
Temperature- afebrile
Pulse Rate- 96 beats/ min
Blood Pressure- 100/70 mm hug
Respiratory Rate- 18 cycles/ min
Spo2- 99%
GASTROINTESTINAL SYSTEM:
ORAL CAVITY
Lips: dry
Teeth: normal
Gums: normal
Tongue: dry
Tonsils: normal
PER ABDOMEN
Inspection:
- Shape- scaphoid
- Umbilicus- central and inverted
- Movements- in accordance with respiration
- No visible pulsation
- No scars, sinuses, engorged veins

Palpation:
- Mild tenderness in all quadrants of abdomen
- No organomegaly
Percussion:
- Tympanic
- Liver dullness elicited in 5th intercostal space.
Auscultation:
- Bowel sounds- present
Investigations:
- Complete blood picture
- Complete urine examination
- GRBS- 102 mg/dl
- Chest X-Ray
- Liver function Test
6.Renal function Test
Provisional Diagnosis:
Acute Gastroenteritis
Treatment:
- IV fluids-NS,RL,DNS-150 ml/hr
- Inj pantop 40 mg IV/ OD
- Inj zofer 2 cc IV TID
- Inj metrogyl 100 ml IV TID- day 1 and day 3
- Vitals monitoring 4 hourly
- GRBS 6 hourly
- Inj monocef 1 gm IV BD- day 1
- TAB doxycycline 100 mg 3 tablets stat
- TAB sporolac DS/ PO/BD
- ORS sachets - 2 in 1 L water, 200 ml after each episode.




Comments
Post a Comment