A 31year old male with alcoholic liver disease
CHIEF COMPLAINT:
A 31 year old male came to the opd with chief complaints of
- Abdominal pain and distension since 7 days
- Pedal edema extending upto knees since 7 days
- Fever since 4 days
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 1 year back then he had pain in abdomen which is of diffuse type(Not associated with vomiting).
He stopped drinking due to the pain and got treated from local RMP for the pain.
After the pain has subsided, ,he started to drink again. He had multiple attacks of pain in the abdomen during the past 1 year.
Two months back he had c/o yellowish discoloration of eyes, pain in the abdomen and b/l pedal edema for which he got treated at NIMS, his symptoms subsided within 2 days.
Then he was tested positive for COVID-19 by RTPCR test, for which he referred to Gandhi hospital and took medication for 10 days and went back home. By that time yellowish discoloration of eyes was still present.
One week back he had non-vegetarian food(mutton) for his dinner, and then developed pain in the abdomen, for which he got treated in the local hospital.
There was insidious onset of Abdominal distension, pedal edema extending upto knees and Fever(Intermitent, low grade, relieved with medication) since 4 days.
HISTORY OF PAST ILLNESS:
Not k/c/o DM, hypertension, asthma, epilepsy, Heart disease or tuberculosis.
He has a treatment history which has been taken for RTA which occurred twice once in 2007 and 2014, where he got treated for head injury in both the cases in 2 different hospitals.
No treatment history for DM, hypertension, asthma, epilepsy, Heart disease or tuberculosis.
PERSONAL HISTORY:
He has been consuming alcohol 180ml/day and smoking 1 pack of cigarette/day since past 10 years.
He had an abstinence from alcohol since 2 months.
GENERAL EXAMINATION:
Patient is conscious.
Icterus is present.
B/L Pedal edema is present.
Absence of pallor, cyanosis, clubbing, lymphadenopathy.
VITALS:
1.Temperature:- 98.4 F
2.Pulse rate: 84 beats per min
3.Respiratory rate: 24 cycles per min
4.BP: 80/60 mm Hg
5.SpO2: 98% @ Room air
6.GRBS: 126mg%
SYSTEMIC EXAMINATION:
CVS:
- S1,S2 heard, no murmurs.
- Normal vesicular breath sounds.
- Abdomen is distended
- No tenderness
- No focal neurological defect.
Course in the hospital:
This is a case of 31 year old male with Chronic Liver Disease with Grade 1 varices with Acute Kidney Injury. Patient was admitted on 14/07/2021. Diagnostic ascitic tap of 1 litre was done and the ascitic fluid was sent for investigation which showed high SAAG and low protein. UGIE showed Grade 1 varices with low grade portal HTN and mild PHG. Patient was treated with Inj. Vit k 10mg, Tab Udiliv 300mg, Tab Rifaximine 550mg, Syp. Hepamerz 10ml, Syp Lactulose, Tab Lasix 20mg, Tab Aldactone 25mg everyday and was advised discharge on 19/7/21.
Advice at Discharge:
1. Tab. Udiliv 300mg PO/BD
2. Tab. Lasix 20mg PO/BD
3. Tab Aldactone 25mg PO/BD
4. Syp Hepamerz 10ml TID
5. Syp Lactulose 15ml
Patient came back again on 6/8/2021 to the opd with the complaints of
- BilateraL Pedal edema Which Is of piting type extending upto knees since 3 days
- No h/o pain abdomen,distension,fever,vomitings,loose stools
- No other complaints
GENERAL EXAMINATION:
Patient is conscious.
Icterus is present.
B/L Pedal edema is present.
Absence of pallor, cyanosis, clubbing, lymphadenopathy.
VITALS:
1.Temperature:- 98.4 F
2.Pulse rate: 92 beats per min
3.Respiratory rate: 24 cycles per min
4.BP: 90/50 mm Hg
5.SpO2: 98% @ Room air
6.GRBS: 126mg%
SYSTEMIC EXAMINATION:
CVS:
- S1,S2 heard, no cardiac murmurs.
- Normal vesicular breath sounds.
- Abdomen is distended
- No tenderness,palpeble masses
- Liver palpeble
- Spleen nt palpeble
- Bowel sounds -yes
- Genitals - normal
- Conscious, speech is normal
- No focal neurological defect.

Discharge DateDate: 08/08/21Ward:MMWUnit:5Name of Treating FacultyDR SAI DEEPIKA (INTERN)DR NIKHILESH KRISHNA (INTERN) DR VAMSI KRISHNA PGY1DR RASHMITHA PGY2DR NIKITHA PGY2DR HAREEN (SR)DR ARJUN KUMAR (AP)DR RAKESH BISWAS (HOD)
DiagnosisCLD WITH LOW GRADE VARICES AND MILD PHG
Case History and Clinical Findings
Patient was apparently asymptomatic 1 year back then he had pain in abdomen which is of diffuse type(Not associated with vomiting).
He stopped drinking due to the pain and got treated from local RMP for the pain.
After the pain has subsided, ,he started to drink again. He had multiple attacks of pain in the abdomen during the past 1 year.
Two months back he had c/o yellowish discoloration of eyes, pain in the abdomen and b/l pedal edema for which he got treated at NIMS, his symptoms subsided within 2 days.
Then he was tested positive for COVID-19 by RTPCR test, for which he referred to Gandhi hospital and took medication for 10 days and went back home. By that time yellowish discoloration of eyes was still present.
One week back he had non-vegetarian food(mutton) for his dinner, and then developed pain in the abdomen, for which he got treated in the local hospital.
20 days back there was insidious onset of Abdominal distension, pedal edema extending upto knees and Fever(Intermitent, low grade, relieved with medication) since 4 days for which he got treated in our hospital
He was asymptomatic for 15 days followed by
C/O PEDAL EDEMA B/L TYPE EXTENDING UPTO KNEES (PITTING TYPE) since 3 daysNO H/O DM/HTN/ASTHMA/EPILEPSY/CAD/TB
WAS A REGULAR ALCOHOL DRINKER SINCE 10 YEARS STOPPED 2 MONTHS BACK REGULAR SMOKER 5-6 PER DAY SINCE 10 YEARS
ON EXAMINATIONVITALS-TEMP- 97.4 FPR- 80 BPMRR- 20 CPMSPO2- 98% AT RAICTERUS - PRESENTOEDEMA OF FEET - PRESENTCVS - S1 S2 HEARD NO MURMURSRS - BAE PRESENT, NO ABNORMALITIESPER ABDOMEN - LIVER PALPABLE NON TENDER - 16 CM CNS - NORMAL
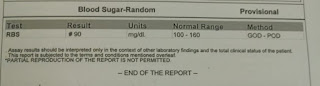
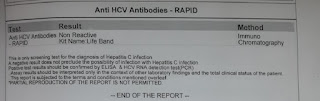
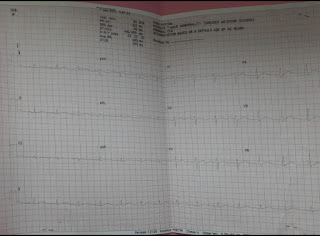
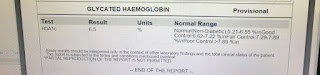
InvestigationCBP RFT LFT ECG USG APTT PT
Investigations
BLOOD UREA 06- 61 mg/dl 42-12 mg/dl 08-2021 12:54:PMSERUM CREATININE 2021 12:54:PM1.2 mg/dl1.3-0.9 mg/dl06-08- COMPLETE BLOOD PICTURE (CBP) 06-08-2021 12:54:PMHAEMOGLOBIN TOTAL COUNTNEUTROPHILS LYMPHOCYTES EOSINOPHILS MONOCYTES BASOPHILS PLATELET COUNT SMEAR7.5 gm/dl28000 cells/cumm86 %06 %02 %06 %00 %4.0Normocytic normochromic anemiawith neutrophilic leucocytosis17.0-13.0 gm/dl 10000-4000 cells/cumm 80-40 %40-20 % 6-1 % 10-2 % 2-0 % LIVER FUNCTION TEST (LFT) 06-08-2021 12:55:PMTotal Bilurubin Direct Bilurubin SGOT(AST) SGPT(ALT) ALKALINEPHOSPHATE TOTAL PROTEINS ALBUMINA/G RATIO13.18 mg/dl 7.16 mg/dl 36 IU/L11 IU/L181 IU/L5.9 gm/dl 2.24 gm/dl 0.611-0 mg/dl 0.2-0.0 mg/dl 35-0 IU/L 45-0 IU/L 128-53 IU/L8.3-6.4 gm/dl 5.2-3.5 gm/dl SERUM ELECTROLYTES (Na, K, C l)06-08-2021 12:55:PM145-136 mEq/L 5.1-3.5 mEq/L 98-107 mEq/LSODIUM POTASSIUM CHLORIDE136 mEq/L 3.8 mEq/L 101 mEq/L Treatment Given(Enter only Generic Name)DAY 1FLUID AND SALT RESTRICTION1) INJ THIAMINE 1 AMP IN 100 ML NS IV / TID 2) INJ VIT K 10 MG IV/OD3) TAB LASIX 40 MG PO/BD4) TAB ALDACTONE 50 MG BD5) TAB PANTOP 40 MG PO/OD6) TAB UDILIV 300 MG PO/BD7) SYP LACTULOSE 15 ML PO/OD8) DAILY WEIGHT AND ABD GIRTH MONITORINGDAY 2FLUID RESTRICTION (LESS THAN 1 L/DAY)SALT RESTRICTION (LESS THAN 2G/DAY)1) INJ VIT K 10 MG IV/OD2) TAB LASIX 40 MG PO/BD3) TAB ALDACTONE 50 MG BD4) TAB PANTOP 40 MG PO/OD5) TAB UDILIV 300 MG PO/BD6) SYP LACTULOSE 15 ML PO/OD7) TAB BENFOMET PLUS OD8) DAILY WEIGHT AND ABD GIRTH MONITORINGAdvice at DischargeFLUID RESTRICTION (LESS THAN 1 L/DAY)SALT RESTRICTION (LESS THAN 2G/DAY)1) INJ VIT K 10 MG IV/OD2) TAB LASIX 40 MG PO/BD3) TAB ALDACTONE 50 MG BD4) TAB PANTOP 40 MG PO/OD5) TAB UDILIV 300 MG PO/BD6) SYP LACTULOSE 15 ML PO/OD7) TAB BENFOMET PLUS ODWhen to Obtain Urgent CareIN CASE OF ANY EMERGENCY IMMEDIATELY CONTACT YOUR CONSULTANT DOCTOR OR ATTEND EMERGENCY DEPARTMENT.Preventive Care



















Comments
Post a Comment