A case of alcoholic liver disease
A 37 year old male came to the OPD with complaints of jaundice since 3 months, with a history of 7 years alcohol intake 360ml/day.
History of generalised weakness and yellowish discolouration of sclera, skin and urine 3 months back for which he went to a local hospital and on routine examination was found to be having deranged LFT.
Symptomatic treatment was given and the patient was advised to stop alcohol.
He improved symptomatically with treatment and the patient continued to take alcohol.
He again had similar complaints for which he came to our hospital.
History of vomitings since 1 month whenever he consumes alcohol.
No history of pain in abdomen, loose stools, pedal edema, abdominal distension/hematemesis.
3 years back history of similar complaints
No known case of DM, hypertension, asthma, epilepsy, CAD, TB
3 days back he consumed 90 ml alcohol along with food intake.
No significant personal and family history - consuming alcohol since 7-8 years, 3 quarters per day.
GENERAL EXAMINATION:-
Icterus+
No pallor, cyanosis, clubbing, lymphadenopathy, edema
VITALS-
Temperature 98.4 F
Pulse rate 74 bpm
RR 16 cycles per min
BP 120/70 mmHg
SPO2 at room AIR - 98%
SYSTEMIC EXAMINATIONJ:-
CVS S1 & S2+
RS NVBS+
Abdomen - scaphoid shaped abdomen, BS+
CNS - patient was conscious, speech normal
Cranial nerves, motor system, sensory system - normal
GCS 15/15
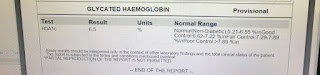
INVESTIGATIONS:-
USG abdomen - Grade 2 fatty liver with altered echo pattern
Few hypoechoic areas in body of pancreas
Gall bladder wall edema with thin layer of pericholecystic fluid - likely acute cholecystitis
Mild ascites
UGIE: Low grade oesophageal varices
3/8/2021 severe PHG
DIAGNOSIS:-
Alcoholic liver disease
Cirrhosis with low grade oesophageal varices, severe PHG
Other investigations done, treatment, advice at discharge and the follow up are shown below:-




Comments
Post a Comment